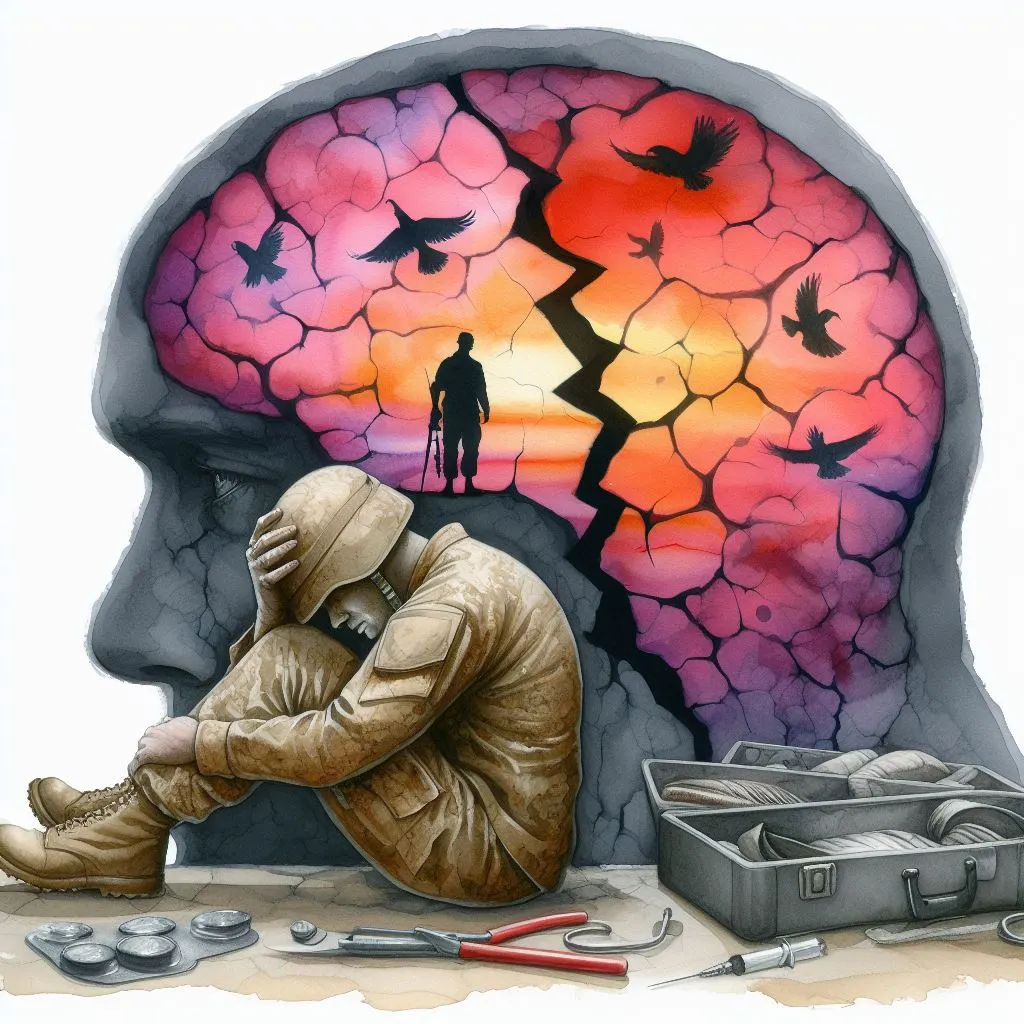
In this comprehensive guide, we delve into the depths of an often misunderstood aspect of trauma and healing – the PTSD fracture. This term is metaphorical, representing the deep psychological splits that traumatic stress can create, akin to how a physical fracture splits bone. Here, you’ll find answers to the most pressing questions surrounding PTSD fractures, from their definition to the path of recovery.
Whether you’re personally affected by PTSD, a caring loved one, or simply seeking knowledge, this article aims to shed light on this complex mental health challenge and guide you through understanding its nuances and the journey toward healing.
What is a ‘PTSD fracture’ and how does it differ from typical PTSD?
A ‘PTSD fracture,’ often used metaphorically, refers to a particularly severe, often complex form of Post-Traumatic Stress Disorder (PTSD) that results from experiencing deeply traumatic events. Unlike typical PTSD, which can stem from a wide range of trauma, a PTSD fracture implies a “breaking point,” where the individual’s ability to cope with stress and trauma becomes overwhelmingly compromised.
Differences between PTSD and a PTSD fracture:
- Complexity: A PTSD fracture may involve multiple, repeated traumatic incidents, making it more complex and harder to treat than PTSD from a single event.
- Symptom Severity: The symptoms are often more intense and can include severe dissociation, where an individual feels detached from reality or themselves.
- Impact on Functioning: It can have a debilitating effect on a person’s daily functioning, sometimes leading to complete disruption of normal life activities.
- Treatment Approach: Due to its complex nature, treating a PTSD fracture often requires a multifaceted approach, including specialized therapies like EMDR (Eye Movement Desensitization and Reprocessing), somatic experiencing, and prolonged exposure therapy.
A discussion on PTSD fractures necessitates an understanding of the profound psychological impact and the often convoluted path to recovery, distinguishing it from more typical forms of PTSD.
Can physical trauma directly lead to PTSD, and how are the two linked?
The direct correlation between physical trauma and PTSD is a subject of significant concern and study. While not every individual who experiences bodily harm will develop PTSD, there’s a substantial risk factor associated with physical injuries, especially when they occur in traumatic contexts such as accidents, combat, or violence.
The link between physical trauma and PTSD:
- Memory Formation: The traumatic event leading to physical injury may be encoded in memory with intense emotion, which can later resurface as flashbacks or nightmares characteristic of PTSD.
- Loss of Safety: Physical trauma often shatters the sense of safety and invulnerability, making individuals more susceptible to PTSD as they struggle with vulnerability and unpredictability.
- Chronic Pain: Ongoing pain or the prolonged process of physical recovery can serve as a constant reminder of the trauma, potentially exacerbating PTSD symptoms.
- Medical Interventions: Invasive medical treatments and hospitalizations can also be traumatic experiences that compound the stress response and contribute to the development of PTSD.
Understanding the intertwining of physical and psychological trauma is fundamental to recognizing and addressing PTSD in individuals who have sustained serious injuries.
What are the common symptoms of a PTSD fracture?
A PTSD fracture typically encompasses a range of debilitating symptoms that may have a profound influence on an individual’s well-being. Recognizing these symptoms is crucial for early intervention and management of the condition.
Common symptoms include:
- Intrusive Memories: These may manifest as distressing recollections, nightmares, or flashbacks of the traumatic events.
- Avoidance: Efforts to avoid thoughts, feelings, conversations, or places associated with the trauma.
- Negative Alterations in Thoughts and Mood: Persistent negative beliefs about oneself or the world, distorted blame of self or others, and a pervasive state of fear, horror, anger, guilt, or shame.
- Alterations in Arousal and Reactivity: This includes being easily startled, feeling tense, having difficulty sleeping, and experiencing angry outbursts, indicative of heightened physiological arousal.
Understanding common symptoms is essential to recognizing a PTSD fracture, encouraging early intervention, and minimizing the long-term impact of the disorder.
How does the diagnosis process for a PTSD fracture work?
Diagnosing a PTSD fracture involves a thorough evaluation by a mental health professional who can differentiate between the nuances of complex PTSD and a PTSD fracture. The process is systematic and empathetic, ensuring accurate diagnosis and subsequent treatment.
The diagnosis of a PTSD fracture may involve:
- Clinical Interview: This is often the first step, where a clinician conducts a detailed interview to understand the history and impact of traumatic experiences.
- Psychological Assessments: These may include standardized questionnaires or scales specifically designed to evaluate the presence and severity of PTSD symptoms.
- Differential Diagnosis: The clinician will consider other mental health conditions that might explain the symptoms, ensuring that the diagnosis of PTSD is precise.
- Observation of Behavior: In some cases, observing the individual’s behavior over a period may provide additional insights that contribute to the diagnosis.
- Collateral Information: Information from family members, friends, or medical records can also play a vital role in corroborating the individual’s account of the trauma and its consequences.
The process for diagnosing a PTSD fracture is meticulous and should be handled with sensitivity considering the complex nature of the disorder.
What treatment options are available for someone with a PTSD fracture?
When it comes to treating a PTSD fracture, a variety of evidence-based options are available, each tailored to address the multifaceted nature of the disorder.
Treatment strategies include:
- Psychotherapy: Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Prolonged Exposure Therapy are some effective modalities.
- Medications: SSRIs and SNRIs are commonly prescribed to alleviate symptoms.
- Complementary Therapies: Activities like yoga, meditation, and acupuncture can support overall well-being and reduce symptoms.
- Support Groups: Connecting with others who have similar experiences can provide solace and understanding.
- Intensive Outpatient Programs: For those who need more structured support, these programs offer a combination of therapeutic interventions.
It is crucial for treatment to be personalized, often involving a combination of these options, to help individuals manage symptoms and work toward recovery.
What are the long-term effects of a PTSD fracture if left untreated?
Without proper treatment, PTSD fractures can lead to persistent and debilitating long-term effects that infiltrate all facets of life.
The enduring repercussions may include:
- Chronic Pain and Health Issues: Stress and anxiety related to PTSD can manifest in physical symptoms and chronic health conditions.
- Substance Abuse: Many individuals may turn to substances as a way to self-medicate and mitigate the distress of PTSD symptoms.
- Relationship Difficulties: The strain on interpersonal connections can result from avoidance, negative mood, and irritability associated with PTSD.
- Occupational Instability: Difficulty concentrating and heightened reactivity can compromise professional performance and lead to job losses.
- Suicidal Ideation: The overwhelming nature of PTSD symptoms increases the risk of suicidal thoughts and behaviors.
Understanding these potential long-term effects underscores the importance of seeking prompt and effective treatment for a PTSD fracture.
How can loved ones support someone with a PTSD fracture?
Supporting someone with a PTSD fracture is a delicate balancing act that requires patience, understanding, and knowledge of the condition.
Here’s how loved ones can help:
- Educate Yourself: Understand what PTSD is and the challenges it presents.
- Listen Without Judgment: Provide a compassionate ear and reassure the individual that their feelings are valid.
- Encourage Professional Help: Gently suggest seeking treatment and offer to assist in the process if needed.
- Maintain Routine and Stability: This can create a sense of security and normalcy for the affected individual.
- Be Patient and Give Space: Recognizing when to give them space and to be patient with their recovery process.
Support from loved ones is a cornerstone of healing and can significantly impact the recovery of someone with a PTSD fracture.
Are there any specific coping strategies for dealing with a PTSD fracture?
Individuals with a PTSD fracture can employ numerous coping strategies to help manage their symptoms and improve their quality of life.
Some effective coping mechanisms are:
- Mindfulness and Relaxation Techniques: Practices like meditation and deep breathing exercises can help regulate the body’s stress response.
- Regular Exercise: Physical activity can act as a natural stress reliever and mood booster.
- Establish a Routine: Consistency in daily activities can provide structure and predictability.
- Healthy Sleep Hygiene: Prioritizing sleep can help manage PTSD symptoms and improve overall health.
- Setting Boundaries: Understanding personal limits and communicating them to others is key to managing stress levels.
Implementing these coping strategies can make a substantial difference in how individuals with a PTSD fracture navigate their symptoms and recovery process.
How does a PTSD fracture impact one’s professional life?
A PTSD fracture can severely impact professional life due to its intense symptoms and the consequent disruption in cognitive and emotional functioning.
The impact may manifest as:
- Reduced Concentration: Difficulties in focusing and memory issues can impair job performance.
- Increased Absenteeism: The need for medical appointments or the inability to cope with stress may result in frequent absences.
- Conflict with Colleagues: Irritability and anger can strain professional relationships and lead to conflict.
- Difficulty Handling Pressure: Stressful situations may evoke strong PTSD responses, making it hard to cope with job demands.
Addressing these professional impacts is crucial for the individual’s overall recovery and well-being.
Is it possible to fully recover from a PTSD fracture?
Recovery from a PTSD fracture, while challenging, is possible with the right approach to treatment and support.
Recovery may involve:
- Sustained Therapy: Ongoing therapy can continue to provide skills and strategies to manage symptoms.
- Building Resilience: Learning adaptive coping mechanisms and strengthening resilience to stress.
- Social Support: A robust support network can be instrumental in recovery.
- Continued Self-Care: Maintaining a healthy lifestyle supports the healing process.
Recovery isn’t necessarily about eliminating all symptoms but rather about regaining control over one’s life and rediscovering a sense of purpose.
Conclusion: Stitching Together the Fractures of Trauma
Navigating the complexities of a PTSD fracture is akin to healing a deep, intricate break. This article has traversed the healing journey, from understanding the nature of a PTSD fracture and its symptoms to the most effective coping strategies and treatments available. Recovery is personal and, at times, trying, but with unwavering support, professional guidance, and resilience, the fractures can be stitched together, leading individuals back to wholeness.
The path is there for those ready to walk it. Should you or a loved one be facing the struggles of a PTSD fracture, remember that help is available, and healing is within reach. Reach out to a healthcare provider, seek support groups, and never underestimate the power of one step forward. Your journey to recovery begins with the courage to ask for help – make that bold step today.